Wagner, S. (2016/2017): Narkosevorbereitung im Kontext von BigData als entscheidende interdisziplinäre Informationsdrehscheibe für die Patientensicherheit in der perioperativen Medizin
Das Projekt „Elektronische perioperative Risikoevaluation“ unter der Leitung von Dr. med. Stefan Wagner, MHBA ist der übergeordnete Rahmen für zwei Teilprojekte aus den Jahren 2016 und 2017:
Ein funktionsfähiger Prototyp wurde erfolgreich nachfolgenden Funktionstests unterzogen:
- Laborbedingungen mit Testdaten
- Anwendertests (Ärzte) mit Test- und Echtdaten.
Electronic support for perioperative risk evaluation – a pilot study and proof of concept
State-of-the art
Main goal of preanaesthetic evaluation is to decrease morbidity and mortality by review of medical history, examination, test results and providing goal-oriented referrals for medical consultations if appropriate and needed. This kind of demanding assessment process precedes surgical and non-surgical procedures that will be carried out under sedation, general or other anaesthesia. In particular, discovery of potential risk factors influences the selection of the anaesthetic technique, essential actions and the necessity of specific anaesthetic postoperative care.
There are different great challenges. Aging population with much comorbidity (such as chronic bronchitis, asthma, diabetes, rheumatism, hypertension, heart failure, renal insufficiency) and multimedication are the most essential ones. The anaesthesiologist visits increasingly elderly patients. More than 50 % of patients older than 65 years take more than 5 drugs per day. Insufficient diagnostic investigations and diagnostic findings serve as catalysts. Linguistic barriers gain more and more influence complicating data collection and anamnesis. Environment conditions like night duty and lacking continuous presence of interpreters during hospital stay complicate the process. Standard operating procedures (SOPs) are consulted to decide on obligatory preoperative diagnostic investigations and to select the best anaesthetic procedure. The flood of data is tremendous. Medical documentation connected with risk evaluation is still tedious despite of the introduction and use of clinical information systems. Daily documentation processes are mainly a combination of many different paper forms and computer applications at the same time for similar or identical information at several medical departments. Thus, anaesthesiologists spend a lot of working time on data collection, filtering for relevant information and taking a sufficient decision based on their medical expertise.
Potential main benefits of electronic health records (EHRs) compared to paper are containment of costs and reduction of errors. Accuracy and completeness of clinical documentation were improved by EHR. More relevant care data could be delivered, too. Decision support raised adherence to guidelines and recommendations. Present anaesthesia clinical decision support contains antibiotic administration timing, improved documentation, timely billing structures, and postoperative nausea and vomiting (PONV) prophylaxis. Up to 30 % suffer from PONV after general anaesthesia. In industrialised countries 20 to 25 % of the population suffer from chronic pain. Acute pain can become chronic pain as well. Supposedly even small operations can lead to chronification of pain. It varies from 3 to 80 %, depending on procedures. Psychological factors and insufficient pain therapy are essential risk factors for chronification. After surgery pain therapy is a core task, becoming even more difficult in cases of chronification. So risk identification and targeted interventions are main aims of the anaesthesiologist. It is obvious that EHR implementations offer opportunities of data-mining to enhance process structures including management, finance and patient care. Clinical decision support is part of the EHR at a very high level. The use of real-time data for decision support and process automation provides the potential to reduce costs and to increase quality of patient care. The objective of decision support (DS) is the supportive modification of clinician behaviour through recommendations of actions and practical advice. However, only a few anaesthesia departments use at least specific EHRs to the needs of anaesthesiology. DS is a great help at many intensive care units.
In Germany more than 16 million operations are performed every year, at Erlangen University Hospital (EUH) alone more than 30.000. For patient safety perioperative risk evaluation is essential. Medication errors or not considered information of medical history, such as allergies or predispositions, are not only in the perioperative area an important cause of morbidity and mortality. The preoperative anaesthesia evaluation comprises comprehensive review of medical records at the hospital as well as paper based information of other healthcare service providers. In addition, all patients have to fill out paper based questionnaires for anaesthesia and surgery. There have been approaches for optimizing this insufficient workflow. For example, patients can fill out an electronic questionnaire at home or use tablets to fill in information about medical history. Electronic questionnaires have proven to provide reliable data. Many hospitals use EHRs and some even special anaesthesia information management systems (AIMS) for preoperative data capture and intraoperative electronic anaesthesia protocols. In 2010 merely 51 % of the university hospitals in Europe used an AIMS. EUH uses the AIMS NarkoData by IMESO since 2001. It includes a preoperative risk evaluation data capture module called NarkoWeb. However, it is merely applicable for manual data input without any further functionality of decision support. Many studies report on the benefits of the introduction of AIMS for data quality of intraoperative anaesthesia documentation. The workload of anaesthesiologists could be decreased accordingly. Increased time for the individual patient is one major advantage. Completeness of anaesthesia records was also evaluated. Previous studies compared user interfaces and usability. Doctors must manage an increased perioperative amount of knowledge, information and data. However, data presentation and filtering to relevancy is mainly unstructured and distributed around the workplace. It is a jungle of computer applications and paper piles. Thus, potentially dangerous information overload could compromise patient safety.
As a result concluding data management is necessary with electronic decision support of risk evaluation. This includes appropriate hierarchical structure and summarising of data. One study reported on the algorithm-based assignment of an ASA score to a completed electronic questionnaire, comparable to the one an experienced doctor would select. AIMS should support integration of new scientific evidence into practice and exchange of complex health information between different hospital departments. These systems will then improve patient safety and outcome. But there is still lack of interoperable solutions in health information systems. Besides, clinicians are rarely involved in implementation planning, design and roll-out as well as evaluation of clinical impacts. Two different preoperative anaesthesia evaluation processes have to be taken into account: Patients come to the anaesthesiological outpatient department at Erlangen University Hospital, in 2016 more than 16.000. In this case doctors extract data manually from paper forms and electronic health records. In a next step manual input into the AIMS is necessary again. If the anaesthesiologist visits patients at the bedside, he has to use a summarizing paper form instead. This information is entered into the AIMS during an operation by another doctor. Computerized systems have shown to require less examination time than manual workflows. It is obvious that vital data could be distorted or even lost. Both possibilities are also very time-consuming. More than 30 per cent of the daily working time of a doctor is spent for documentation. There is still a remarkable gap between existing information in EHR and data collection processes of identical or similar data. Previous research evaluated helpful integration of personal digital assistants (PDAs) to replace redundant paper documentation. It was proved that PDAs could support the establishment of a complete digital anaesthesiological documentation. At the moment, patients and doctors at EUH have to document information multiple times in different health information systems and on paper. Surgery and anaesthesiology use nearly the same information for informed consent before medical interventions. Both show many similarities in preoperative informed consent, for example pre-existing diseases, allergies and the use of drugs. However, these are not considered in current clinical and data processing procedures.
At the moment these potential synergisms are not used for optimizing the medical workflow for the benefits of staff and patients. But the company „BAVARIAN health“ provides a combined surgical und anaesthesiological informed consent with the software „MEDePORT“. Information films, texts and medical questionnaires are composed individually for one patient and a special procedure. The patient is able to watch the movies with subtitles in his native language, to read the explaining texts in his mother tongue and to fill out the questionnaires digitally ahead of the patient-doctor-communication. Uncertainties and outstanding issues are addressed additional to risk disclosure. It can be used on workstations or tablets. The completed form is signed electronically and stored in the EHR. Moreover, mobile questionnaires proved to be well accepted by users and cost-efficient compared to paper forms. But it does not provide any decision support aiming to select the best anaesthetic procedures, to display recommendations on long-term medication for an individual patient nor help of risk identification. Medication can interact with anaesthetic drugs and could potentially cause morbidity and mortality. Therefore a significant gap in previous research, with only single solutions, can be identified: Comprehensive electronic assistance is not yet available for perioperative risk evaluation.
Bibliography concerning state of the art and the research objectives
Ammenwerth, E./Spötl, H.-P. (2009): The Time Needed for Clinical Documentation versus Direct Patient Care. A Work-sampling Analysis of Physicians’ Activities. In: Methods of information in medicine 48, 1 (2009), S. 84-91.
Arias, A./Benítez, S./Canosa, D./Borbolla, D./Staccia, G./Plazzotta, F./Casais, M./Michelangelo, H./Luna, D./Bernaldo de Quirós, F. G. (2010): Computerization of a Preanaesthesiologic Evaluation and User Satisfaction Evaluation. In: Studies in Health Technology and Informatics 160, 2 (2010), S. 1197-2001.
Balust, J./Egger Halbeis, C. B./Macario, A. (2010): Prevalence of Anaesthesia Information Management Systems in University-Affiliated Hospitals in Europe. In: European Journal of Anaesthesiology 27, 2 (2010), S. 202-208.
Benson, M./Junger, A./Quinzio, L./Fuchs, C./Sciuk, G./Michel, A./Marquardt, K./Hempelmann, G. (2000): Clinical and Practical Requirements of Online Software for Anesthesia Documentation an Experience Report. In: International Journal of Medical Informatics 57, 2-3 (2000), S. 155-164.
Braaf, S./Riley, R./Manias, E. (2015): Failures in Communication through Documents and Documentation across the Perioperative Pathway. In: Journal of Clinical Nursing 24, 13-14 (2015), S. 1874-1884.
Fuchs, C./Quinzio, L./Benson, M./Michel, A./Rohrig, R./Quinzio, B./Hempelmann, G. (2006): Integration of a handheld based anaesthesia rounding system into an anaesthesia information management system. In: International Journal of Medical Informatics 75, 7 (2006): S. 553-563.
Goodhart, I. M./Andrzejowski, J. C./Jones, G. L./Berthoud, M./Dennis, A./Mills, G. H./Radley, S. C. (2017): Patient-completed, preoperative web-based anaesthetic assessment questionnaire (electronic Personal Assessment Questionnaire PreOperative): Development and validation. In: European Journal of Anaesthesiology 34, 4 (2017): S. 221-228.
Springman, S. R. (2011): Integration of the Enterprise Electronic Health Record and Anesthesia Information Management Systems. In: Anesthesiology Clinics 29, 3 (2011), S. 455-483.
Stabile, M./Cooper, L. (2013): Review Article: the Evolving Role of Information Technology in Perioperative Patient Safety. In: Canadian Journal of Anaesthesia 60, 2 (2013), S. 119-126.
Trentman, T. L./Mueller, J. T./Ruskin, K. J./Noble, B. N./Doyle, C. A. (2011): Adoption of Anesthesia Information Management Systems by US Anesthesiologists. In: Journal of Clinical Monitoring and Computing 25, 2 (2011), S.129-135.
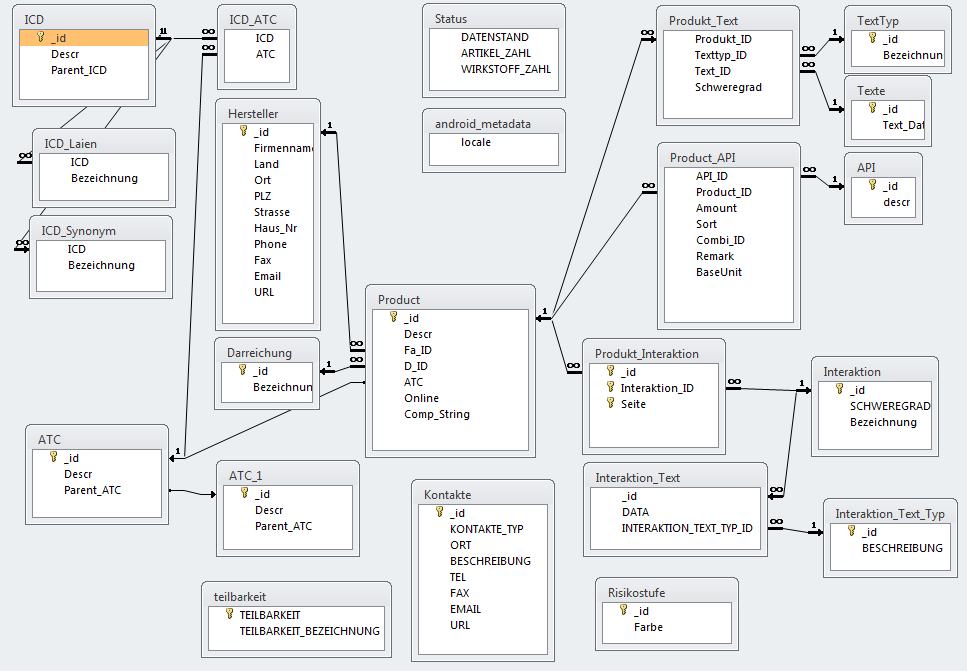
Arzneimittel-Datenbank für automatisierten Interaktionscheck
- ATC: Anatomisch-Therapeutisch-Chemisches Klassifikationssystem zur Einordnung von Medikamenten
- ICD: International Classification of Diseases and Related Health Problems